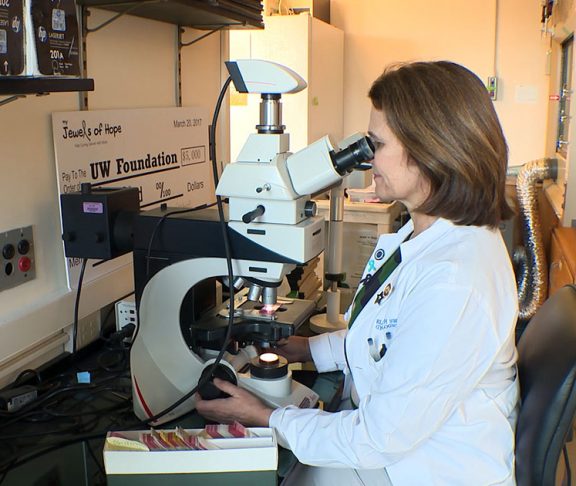
Elizabeth Swisher, MD
Co-leader, SU2C–Ovarian Cancer Research Alliance–National Ovarian Cancer Coalition Ovarian Cancer Dream Team
The COVID-19 pandemic has prompted a dramatic shift in the delivery of healthcare, as medical providers across the United States have pivoted to meet the unprecedented challenges of the pandemic, while also providing the best possible care for all patients. One positive result has been the increased adoption of remote methods for patient care.
One negative result is that many non-urgent appointments, such as preventative cancer screenings, were put on hold at the onset of stay-at-home orders in March in order to conserve essential medical resources and to reduce possible exposure to the virus.
Some of the screenings that have declined the most are critical to women’s health, such as breast and cervical cancer screenings. Routine cancer screenings are vital to cancer prevention and can save lives. As stay-at-home orders relax in many parts of the country, medical centers have resumed routine screenings and patients are encouraged to ask their physician if cancer screening is right for them at this time.
But even before the pandemic, many people didn’t get recommended cancer screenings. Similarly, studies have shown that many people who might have a genetic risk for cancer don’t get tested. These types of tests can often catch the five to 10 percent of breast cancer cases and 20 percent of ovarian cancer cases that are hereditary. These cancers can be very deadly if diagnosed at a later stage, but they are often preventable if the risk is identified before cancer forms.
So why don’t people typically get genetic testing for inherited cancer risk?
Barriers to access
The standard model for genetic testing is simply too burdensome. The process involves a referral to a genetic counselor, an in-person visit with the counselor before the test, a blood draw or spit test in a lab, then another appointment with the counselor to get the results. And this whole process relies on a doctor or the patient identifying the familial risk in the first place. There are too many barriers for this to work for everyone. People may not have the time, transportation, work leave, childcare, or other considerations to go through the whole process.
This process was developed to ensure that patients have enough information as they go through genetic testing. But that paradigm evolved without any real data validating the benefit to patients. That’s why a Stand Up To Cancer ‘Dream Team’ of researchers co-funded by Ovarian Cancer Research Alliance and National Ovarian Cancer Coalition have tested a possible solution through a clinical trial called MAGENTA (Making GENetic Testing Accessible).
A game-changing trial
Nearly 4,000 women from across the United States participated in MAGENTA. Participants had a family history of breast or ovarian cancer or had a family member with a known genetic mutation. Each participant was tested for 19 genetic mutations associated with risk for ovarian, breast, and other cancers. Testing was done from the comfort and safety of participants’ homes using a saliva kit provided by Color Genomics, which was mailed to each participant’s home and returned by standard mail.
Trial participants were split into four groups. In every group, women watched an educational video on genetic testing for cancer risk before completing their test. In the standard group women had mandatory genetic counseling by phone before and after testing. In the other three groups women skipped the pre-test counseling, the post-test counseling, or both. Anyone with a positive test result had genetic counseling delivered by a telephone appointment.
Based on follow-up surveys, the study showed that the electronic genetic education methods were effective and skipping personalized counseling didn’t increase patients’ distress.
Results from the MAGENTA trial provide a foundation for electronic access to genetic testing for cancer risk, with equivalent patient outcomes, less hassle for patients, and less cost to the healthcare system. This type of virtual healthcare makes care accessible and gives people the information they need in the convenience of their own home.
Leveraging lessons learned from the COVID-19 pandemic, let’s embrace a new genetic testing paradigm for cancer risk and empower more people to make important choices to decrease their risk of cancer.