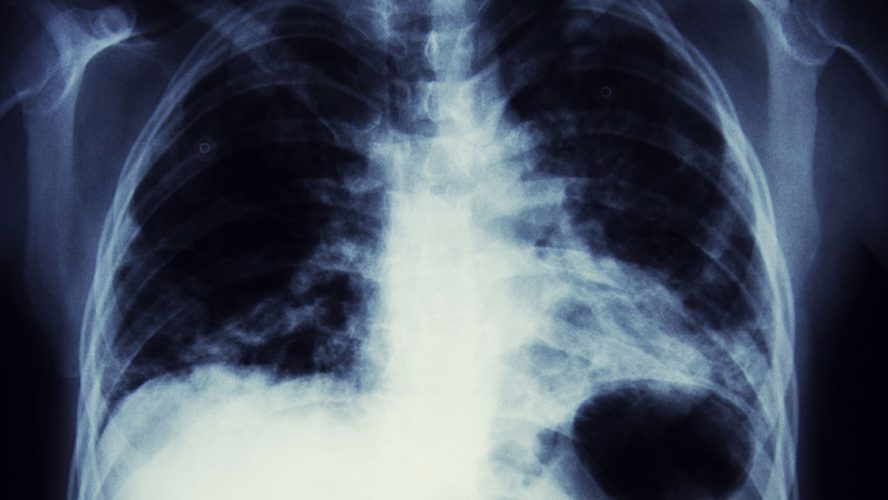
Lung cancer is the No. 1 cancer killer of both men and women, killing more people each year than colon, breast, and prostate cancers combined. One of the reasons it’s so deadly is because early stage lung cancer often doesn’t have symptoms. Only 16 percent of people with lung cancer are diagnosed before the cancer spreads, and once that happens, the five-year survival rate is very low.
Early screening
Physicians have been hoping to improve some of the grim statistics by implementing low-dose CT scanning programs. They are currently the only approved way to screen for the disease – and are able to detect lung cancer in its early stages when there are few, if any, symptoms. Yearly, low-dose CT scans reduced lung cancer deaths among high risk patients by 20 percent, according to the National Cancer Institute’s Lung Screening Trial in 2011.
This type of regular CT screening is available for people without lung cancer symptoms who are 55-77 years old, are a smoker or someone who quit smoking less than 15 years ago, have a smoking history of at least 30 pack years, and are healthy enough to tolerate curative treatment for early stage lung cancer.
There are risks to lung cancer screening. In about 25 percent of people who get screened, small spots on the lungs are found called nodules. The good news is that 95 percent of these nodules are benign scars in the lungs. While most of these nodules are not cancerous, some will require additional tests. This has led to some innovations in testing, including one called microcoil localization.
Microcoil localization
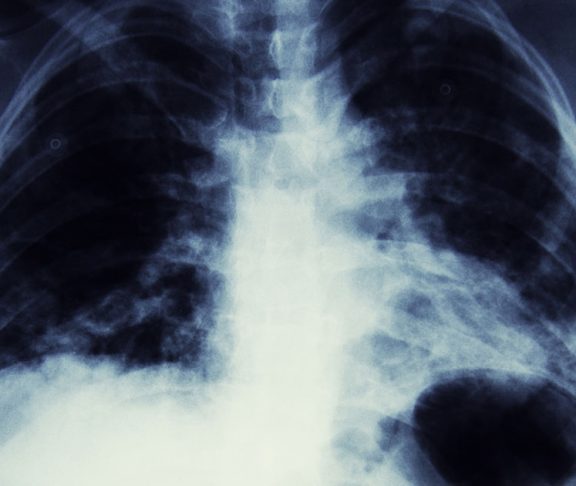
Due to lung cancer screening becoming more widely used, more nodules are being discovered. Until recently, if nodules suspected to be cancer were found the options were to watch and wait to see if the nodule grows, or remove an entire lobe of the lung. Now, a handful of centers across the country are performing minimally invasive microcoil localization.
Using the hybrid operating room CT scanner, a needle pre-loaded with a soft, fiber-coated platinum is threaded through the chest wall, through the lung, and finally into the target nodule. This coil is carefully anchored to the nodule before the needle is removed. Then, a thoracic surgeon – using video-assisted thoracoscopic technology (VATS) – locates the coil on the pleural (membrane around the lungs) surface, and carefully removes it along with the wedge of tissue containing the small nodule or lesion. The team can then instantly examine the tissue, make a diagnosis and perform further surgical treatment, if necessary.
This provides physicians with a minimally invasive diagnostic technique for small lung lesions that were formerly only able to be observed or were only accessible by large incisions associated with significantly more pain and a lengthy recovery. Now, they’re able to assess the nodule more quickly and treat patients with early-stage lung cancers quickly and thus decrease the chance of the cancer spreading.
As lung cancer screening and treatment continue to evolve, your doctor can help you decide what is right for you.